TREATING
HEAVY PERIODS
(HEAVY MENSTRUAL BLEEDING)

WHAT IS HEAVY MENSTRUAL BLEEDING (HMB)?
A useful definition of HMB is when your periods are so heavy that they interfere with your quality of life or your ability to carry out day-to-day activities.1,2
Periods are a normal part of life and if you have always had heavy periods you may think this is normal, but if they’re so heavy that you have to take time off work or school, or can’t do the things you normally enjoy, it’s time to speak to your doctor.
HOW DO I KNOW IF I HAVE HMB?
Think about the impact that your periods have on your life. If you answer ‘yes’ to any of these questions, you could have HMB:1,2,4
- I bleed so much that I have to change my pad/tampon/menstrual cup every 1-2 hours
- I need to use two types of period products (e.g. a tampon and a pad) at the same time
- My periods last longer than 8 days
- I pass large clots during my period
- I have had problems with “flooding” when I bleed through to my clothes
- I need to get up in the night to change my pad/tampon or I have to wear a nappy, put a towel in my bed or use large maternity pads when I sleep
- My period is so heavy that it stops me from doing physical activities like going to the gym, cycling, swimming, etc
- My period is so heavy that it sometimes stops me from going to work or social events
WHAT CAUSES HMB?
HMB can be caused by a lot of different things. Hormonal changes – for
example leading up to the menopause – are a common cause of HMB.5
Other potential causes include:2
- Gynaecological problems such as uterine polyps or fibroids, endometriosis, pelvic infections or endometrial hyperplasia
- Blood disorders which prevent clotting
- Certain medical treatments such as the copper intrauterine device (IUD) or anticoagulant medicines
Some causes of HMB can be identified through medical investigations, but often no definite explanation can be found.2,5,6
It is important to speak to your doctor if your period is so heavy that it makes it difficult for you to do your normal daily activities, or if you have any other concerns about your periods. Even if no obvious reason for your HMB can be found – which is often the case – there are still effective treatments available.
WHAT CAN I EXPECT WHEN I TALK TO MY DOCTOR ABOUT HMB?2-6
Your doctor may ask you questions about your periods and any other symptoms you have or any medications you are taking. They may also ask other questions about your health and sexual history to try and get some clues about what might be causing your HMB.
Your doctor may also need to do a physical examination. This may include (with your consent) an internal examination of your vagina and cervix and what is called a ‘bimanual examination’ of your uterus (womb) to look for any abnormalities. This will involve your doctor placing their fingers inside your vagina to feel your uterus. You may also need to have other tests or scans if an underlying cause is suspected.
WHAT TREATMENTS ARE AVAILABLE FOR HMB?
If no underlying cause is suspected or found, your doctor may recommend certain common medical or surgical treatments to reduce or stop your heavy bleeding and/or manage other symptoms.
Medical treatments include:
An intrauterine system
(also called a ‘hormonal IUD’), known by the brand name Mirena® (52 mg levonorgestrel intrauterine contraceptive device). A small T-shaped device inserted into the uterus by a healthcare professional. It can stay in place for up to 5 years and also provides contraception.
Oral hormonal pills
such as combined oral contraceptive
pills or pills that contain a specific type
of progestogen.
Non-hormonal treatments
such as tranexamic acid or mefenamic acid.
HMB treatment may depend on whether you are currently trying to get pregnant or plan to have children in the future. Discuss all your options with your doctor to decide whether you would like treatment and if so, which treatment would be best for you.
HOW DOES MIRENA® WORK TO HELP REDUCE HMB?
Typically, this is how your period works:7
- Every month, the lining of your uterus thickens during the first half of your menstrual cycle to prepare for ovulation (release of an egg)
- If ovulation takes place and the egg is not fertilized, the uterus sheds its lining. The blood and tissue from the lining of your uterus passes out of your body through your vagina. This is known as your period
- On average, a woman’s period lasts around 5 days. It may be shorter or longer, depending on the woman
- As well as vaginal bleeding, some women experience pain/discomfort and/or changes in mood around the time of their period
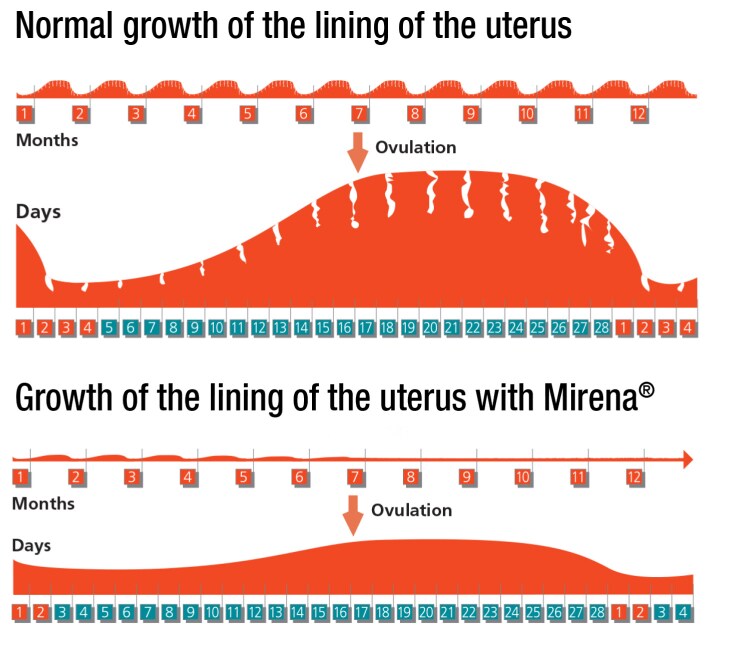
Mirena® can reduce your menstrual bleeding by thinning the lining of the uterus. In a clinical trial in women with HMB and treated with Mirena®, blood loss was reduced by up to 95% at the end of 6 months of use.8,9 Mirena® may also reduce the period pain/discomfort that some women have during their period.8
WHAT OTHER EFFECTS MIGHT MIRENA® HAVE ON MY PERIODS?
You may notice an initial increase in the number of spotting and bleeding days which then typically decrease in the months that follow. Your bleeding may also be irregular.8
Your total blood loss per period may progressively decrease with continued use and you may stop bleeding altogether.8
Contact your healthcare professional if your bleeding remains heavier than usual or increases after it has been light for a while.
Mirena® is very effective at preventing pregnancy but if you have any concerns that you may be pregnant while using Mirena®, contact your healthcare professional without delay.
Want to learn more about Mirena®? View the patient information booklet here
MORE INFORMATION
For more information about HMB speak to your healthcare professional or download the patient booklet.
Talk to your healthcare professional
References: 1. RANZCOG. https://ranzcog.edu.au/womens-health/patient-information-resources/heavy-menstrual-bleeding; accessed May 2022. 2. Health Navigator. https://www.healthnavigator.org.nz/health-a-z/p/periods-heavy-bleeding/; accessed May 2022. 3. Heavy Menstrual Bleeding Clinical Care Standard. Australian Commission on Safety and Quality in Healthcare. October 2017. 4. BPAC NZ. Investigating and Managing Abnormal Vaginal Bleeding: An overview. https://bpac.org.nz/2019/bleeding.aspx; accessed May 2022. 5. Jean Hailes. Heavy menstrual bleeding - Fact sheet. https://www.jeanhailes.org.au/resources/heavy-menstrual-bleeding-fact-sheet; accessed May 2022. 6. Patient. Heavy periods: Menorrhagia. https://patient.info/womens-health/periods-and-periodproblems/heavy-periodsmenorrhagia; accessed May 2022. 7. Healthify He Puna Waiora – Menstruation. https://healthify.nz/health-a-z/m/menstruation/; accessed August 2023. 8. Mirena® Data Sheet, 19 October 2021. 9. Reid PC, et al. BJOG. 2005. 112(8):1121-1125.
MIRENA® (levonorgestrel). MIRENA® is an intrauterine system containing 52 mg levonorgestrel, which is slowly released over 5 years at an initial rate of 20 mcg/24 hours. MIRENA is a Prescription Medicine for contraception. MIRENA is also a treatment for unexplained heavy menstrual bleeding where no underlying pathology causing excessive bleeding can be found and provides protection of the lining of the womb when oestrogen therapy is prescribed for menopausal symptoms. MIRENA must not be used during pregnancy, if there is any sign of pelvic or genital tract infection, inflammation or cancer, if there is womb or cervical abnormality, confirmed or suspected hormone-sensitive cancer including breast cancer, undiagnosed abnormal bleeding, active liver disease or if you are allergic to any ingredients in MIRENA. MIRENA should be inserted by a doctor who has been trained in the insertion technique. Removal of MIRENA is recommended if the following medical conditions occur: an increased susceptibility to infections, acute infection not responding to treatment. Migraine or severe headaches, jaundice, increased blood pressure, hormone-sensitive cancer, stroke, severe heart or blood vessel disease, blood clots may occur during MIRENA use, should this happen; your doctor may consider removal of MIRENA. MIRENA should be used with caution if you have diabetes or a heart condition from birth and are at risk of infection. MIRENA must be removed if pregnancy (which might be outside the womb) or puncture of the womb is suspected or if MIRENA is partially expelled. MIRENA does not protect against HIV infections (AIDS) and other sexually transmitted infections. The pattern of side effects, which are more common in the first months of use, should be explained to you. Commonly reported side effects include changes to menstrual patterns, painful menstruation, genital discharge, redness, or itching, headache/migraine, abdominal, breast or back pain, depressed mood, nervousness, nausea, acne, weight changes, decreased libido, excessive hair growth, benign ovarian cysts and expelled device. The possibility of side effects such as puncture of the womb, allergic reactions, bacterial infection of the blood, breast cancer, or pregnancy outside the womb should be discussed with your doctor, pharmacist or health professional. If symptoms persist or you have side effects, see your doctor for advice. MIRENA is a fully funded medicine – a pharmacy charge and normal Doctor’s visit fees and insertion fees may apply. MIRENA has both risks and benefits. Use only as directed. Consult your doctor to see if MIRENA is right for you. For more information, read the Consumer Medicine Information available at https://www.medsafe.govt.nz/Consumers/cmi/m/Mirena.pdf Bayer New Zealand Limited, PO Box 2825, Shortland Street, Auckland 1140, telephone 0800 229 376.
Mirena® is a registered trademark of the Bayer Group, Germany.
PP-PF-WHC-NZ-0038-2. TAPS NP18704.
